Garner’s turnkey solution modernizes health plan performance by delivering better provider rankings, more accurate directories, and dynamic benefit design—without disrupting networks, filings, or administration.
For Health Plans
Win employer business and improve plan performance — without disrupting your infrastructure
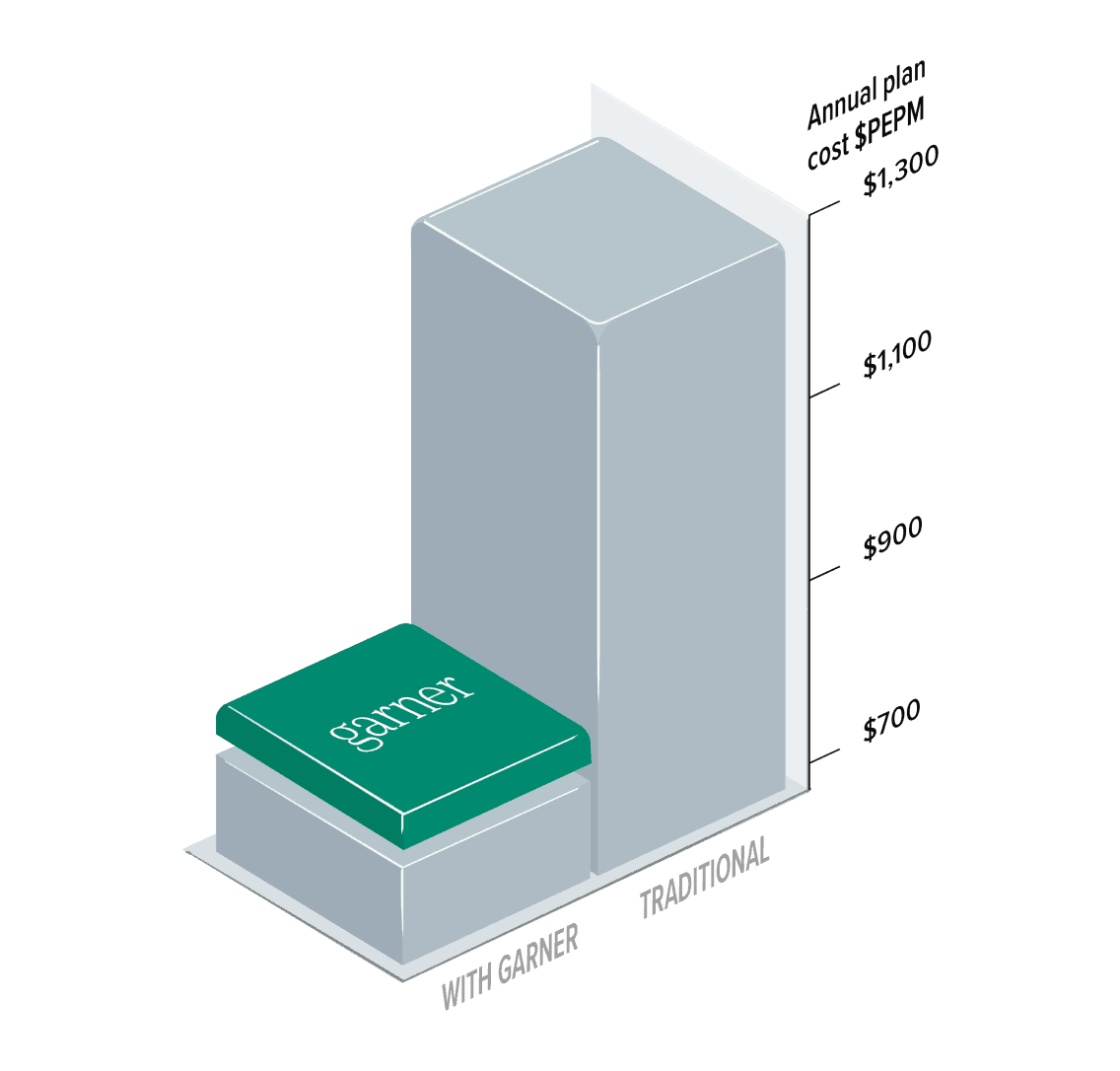
Unlock meaningful savings with a proven incentive model
Garner pairs best-in-class provider rankings with an innovative incentive account that encourages members to choose high-value care.
This approach enables health plans to offer richer benefit designs (including first-dollar coverage options), lower total plan costs by 8–15%, and improve underwriting margin and renewal competitiveness.

Zero disruption to your health plan
Garner works with your existing plans and provider networks, requiring no custom integrations or operational changes. The solution is fully compliant with payer–provider contracts and does not require refiling medical plans.
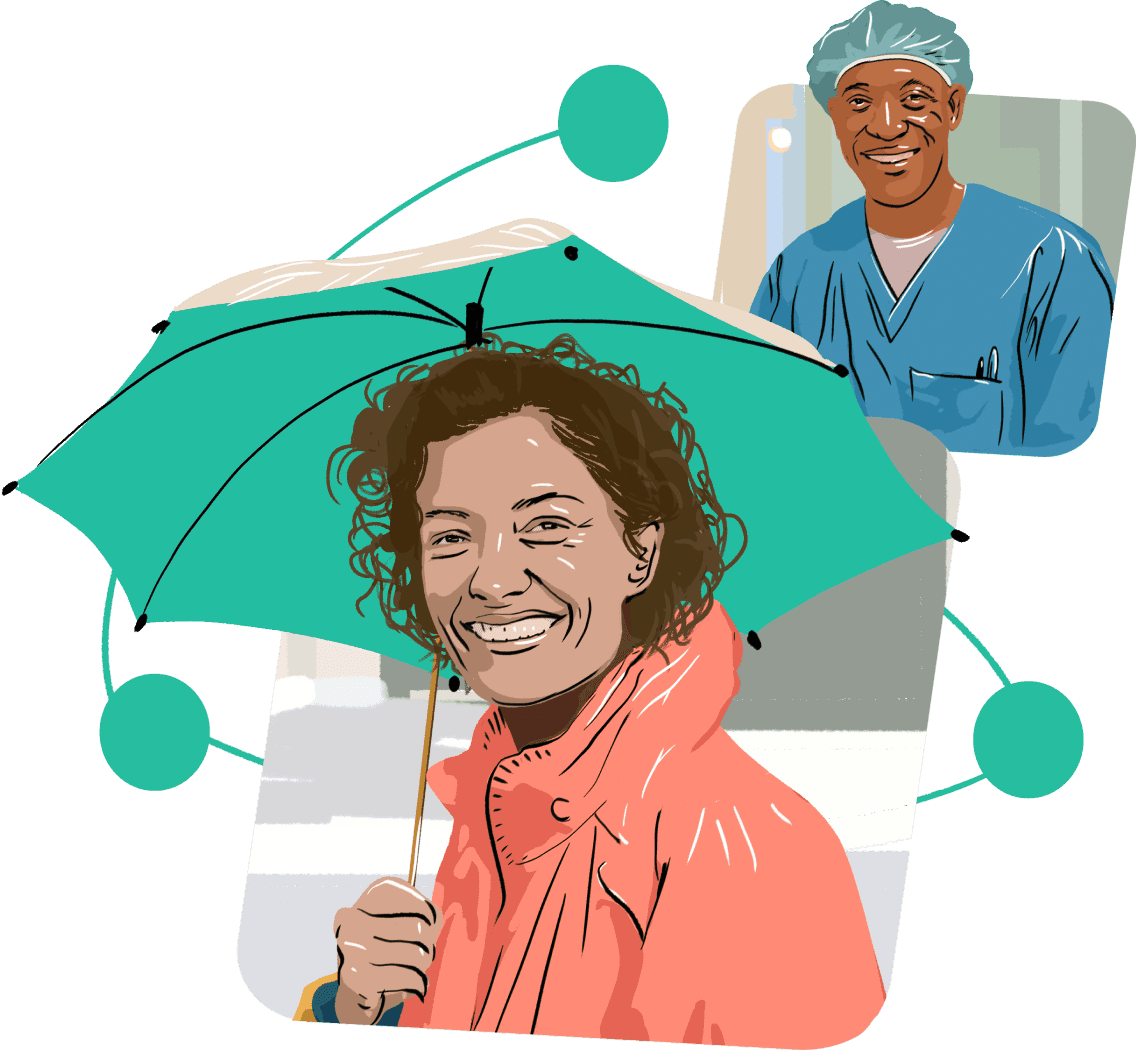
Unmatched member experience
By solving directory issues and taking the guesswork out of finding high-quality care, Garner offers an unmatched experience for health plan members.

Identify high-impact employer opportunities
Use Garner’s claims-based insights to identify employer groups with rising trend, renewal pressure, or opportunity for alternative plan designs.
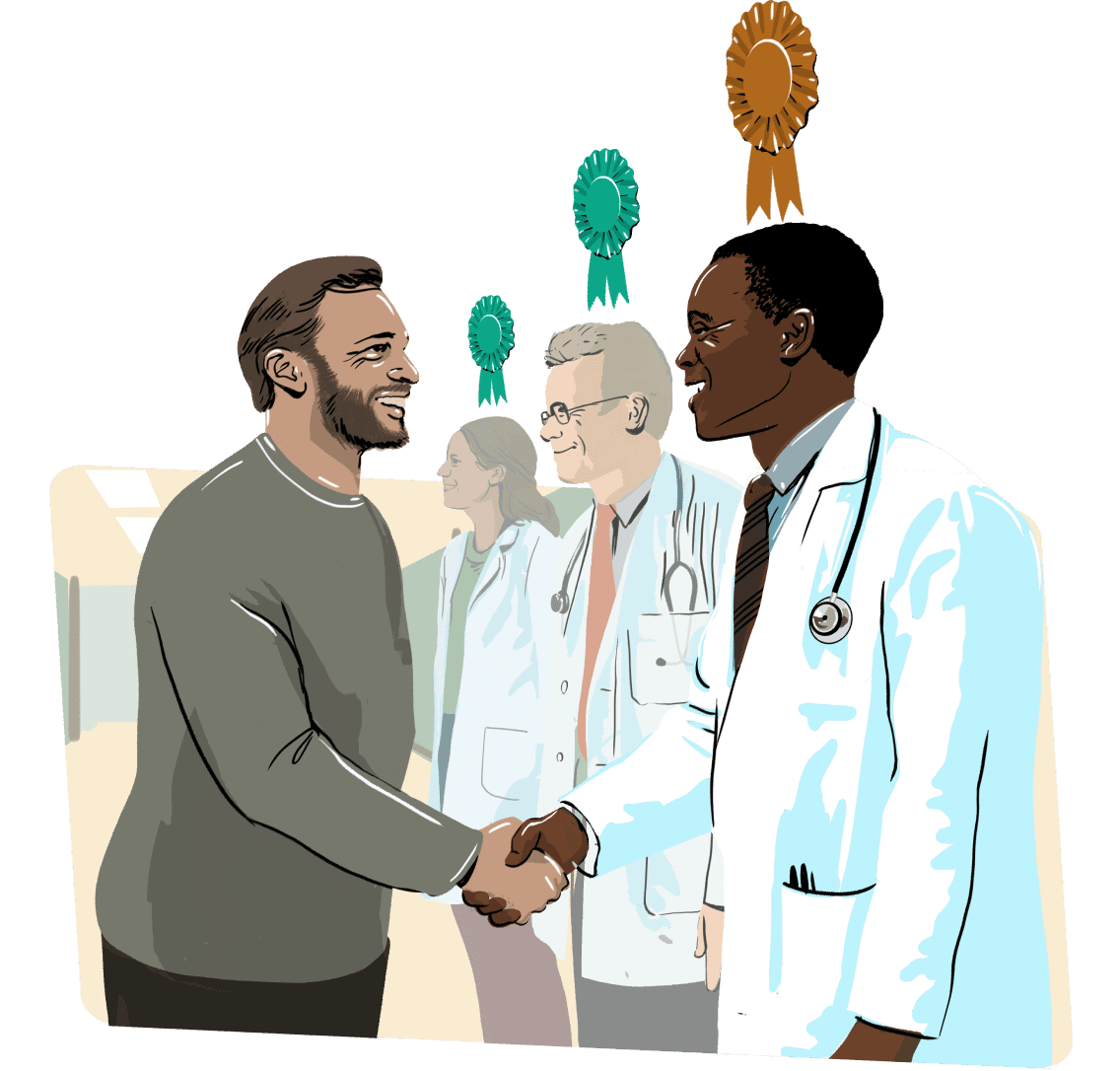
Enhance existing plans — without disruption
Layer Garner onto existing plans and provider networks to enable richer benefit designs and meaningful incentives for high-value care — with no changes to plan filings, networks, or administration.

Improve plan performance and competitiveness
By steering care to top-performing providers, Garner helps health plans lower total cost of care, improve underwriting margin, and deliver more competitive renewals over time.
Garner’s analytics are broader and deeper than any individual plan
Patients in dataset 320+ million 75 million |
# of specialities ranked 82 17 |
# of individual metrics 550+ 73 |
Average member engagement rate 60% 25% |